The best diets for PCOS
Diet is one of the most effective management tools for PCOS. For people suffering from PCOS, dietary changes can efficiently treat unwanted symptoms, such as infertility or hair growth, and help to prevent long term risks, such as diabetes and cardiovascular disease. Diets tailored to PCOS management have four cornerstones: weight management, reduction of insulin resistance, increasing intake of certain nutrients, and avoiding certain harmful food products. In this article we explore the importance of diet, which diets are best for managing PCOS and which foods should be avoided for PCOS management.
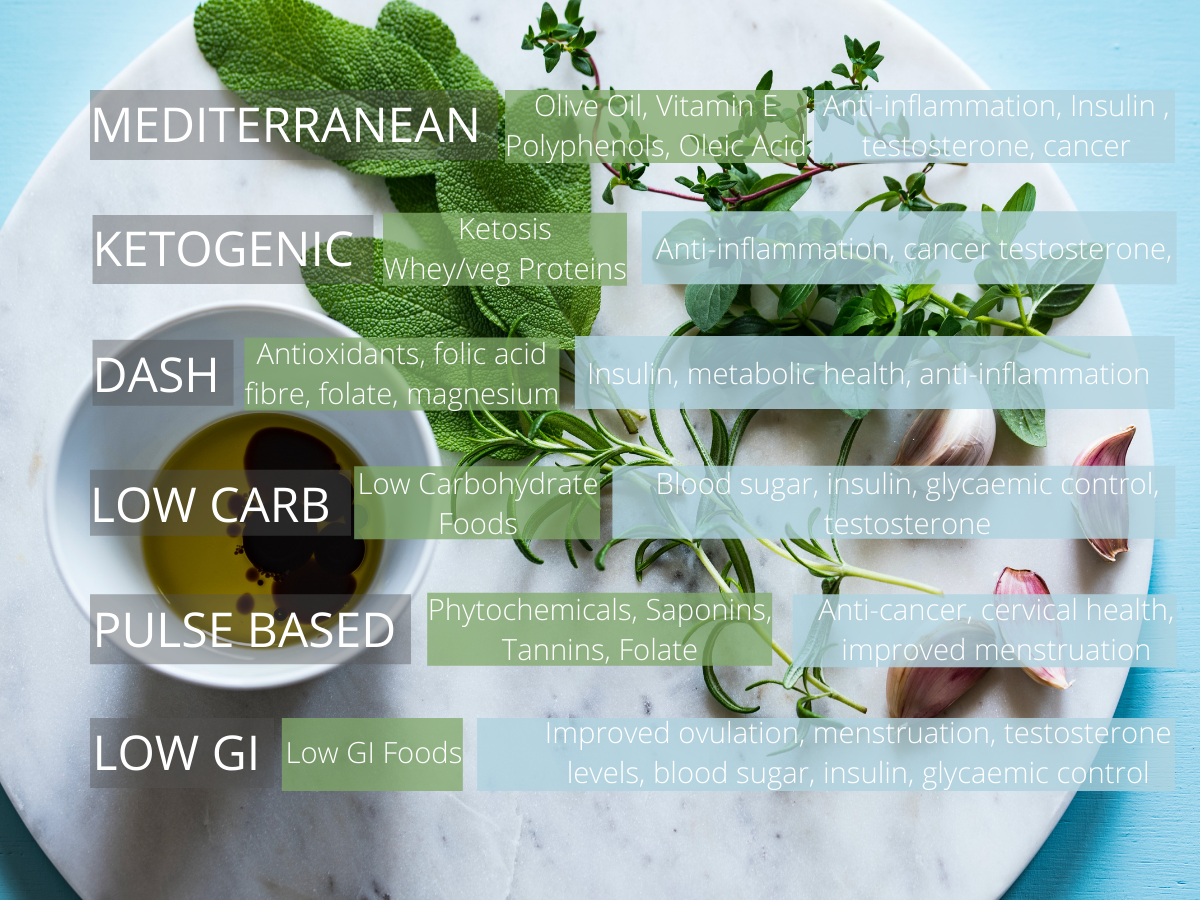
Research has identified these 6 diets as being the best for managing PCOS due to their health promoting components which directly benefit PCOS
Contents
Why is diet important for PCOS?
PCOS is a complex disease, meaning that it has no single cause. Its development is affected by a variety of internal factors, such as genetics, and external factors, such as obesity or chemicals in the diet. For approximately 70% of people suffering from PCOS, the root cause can be traced to insulin resistance, and the symptoms of PCOS are made significantly worse by weight gain. For most other women with PCOS, their symptoms are caused by disruption in the way that their brain produces Luteinising Hormone and Follicle Stimulating Hormone, which can also be greatly worsened by obesity.
Insulin resistance, obesity, hormone levels, and a wide variety of other “markers” of PCOS can all be deeply affected by diet and nutrition. Poor diet and nutrition can result in severely worsened symptoms of PCOS in a number of ways. Poor diet can lead to excess insulin production, which increases insulin resistance and leads to higher testosterone production. Similarly, excess calory intake can lead to high levels of body fat and obesity, which can also worsen insulin resistance. Additionally, some chemicals in the diet can disrupt hormonal balances in the body, which may lead to excess testosterone production by the ovaries and disruption of LH and FSH production in the brain.
To understand more about why insulin resistance and obesity is so important to PCOS, check out: PCOS, Insulin, and Obesity: Everything you need to know.
On the other hand, a healthy diet can help to fix the root cause of PCOS and its symptoms by improving insulin sensitivity and restoring normal hormonal function. This is why diet is considered such an incredibly important tool for the management of PCOS in the short and long term. Studies have found that improving diet in women with PCOS improves menstrual cycle regularity, ovulation and fertility, and symptoms of high testosterone like acne and hair growth. It can also greatly reduce the long term risk of developing diseases like diabetes, cardiovascular disease and endometrial cancer. In fact, one study looking at the effects of a 2-5% weight loss on fertility in PCOS found that half of the women achieved normal ovulation and 2 of them actually conceived during the study! To put that in perspective, that’s the same as a 70 kg / 154 lbs woman losing between 1.4-3.5 kg / 3-7.7 lbs [source].
What kind of diet is best for PCOS?
All women with PCOS should have largely similar goals with their diets, however there are some important distinctions! For PCOS sufferers who are obese, improved diet can result in weight loss and bodyfat loss, which will lead to improved insulin sensitivity and ultimately restoration of hormone levels such as testosterone, LH and FSH. For these women, weight loss and insulin resistance are the core focus of the diet. Many women who suffer from PCOS display insulin resistance but are not obese. For these women, weight loss is not an option however dietary changes focusing on improved insulin resistance should be the goal. Other women suffering from PCOS without obesity or insulin resistance should tailor their diet to avoid unwanted chemicals, maximise intake of important vitamins and minerals, and reduce inflammation as much as possible, in order to restore normal hormonal production [source].
Without any doubt, the single most important factor of a diet for PCOS is that it is sustainable. PCOS must be managed in the long term, in other words, until menopause. For this reason, a diet that lasts for 6 months before the person is unable to continue the diet because they dislike it, or it is too difficult, is entirely unsuitable. A flexible, enjoyable diet that can be used indefinitely will be far more effective in the long term.
So, what is the best diet for PCOS? Many different dietary interventions have been studied in the context of treating and improving PCOS and 6 distinct diets in particular have been identified as being potentially optimal for managing PCOS: the Mediterranean diet, the ketogenic diet, the DASH diet, the low-GI diet, the pulse based diet, and the low carb diet. In addition to these 6, calorie restriction diets are essential for obese or overweight women with PCOS [source].
Best diet for weight loss with PCOS
“A calorie deficit is essential for weight loss”
Hundreds or thousands of diets and concepts have been proposed over the years for weight loss and whilst some of them have scientific evidence to support them, there is only one common factor that all research agrees on as essential for losing weight: calorie deficit.
So, what is a calorie deficit? Simply put, it is when your body is expending more energy than it takes in, forcing it to draw upon the energy that it has previously stored as body fat. Over time, this results in weight loss as your body consumes the stored energy. The rate of weight loss will depend on the size of the calorie deficit. In other words, the greater the difference between intake and expenditure, the faster the weight loss. However, if a deficit is too big not only will daily function become difficult, but the diet may become dangerous. Weight loss will continue until calorie intake is readjusted to “maintenance level”, where calorie intake and calorie expenditure are equal [source].
A calorie deficit can be achieved in two ways. Either the number of calories taken in is reduced (by eating less), or the number of calories spent is increased (by doing more). By combining eating less and exercising, we can integrate the two. Any calorie deficit will induce weight loss, but most research recommends a calorie deficit of between 500-700 calories per day [source].
Research has shown that there is no baseline metabolic difference between healthy women and women with PCOS. For that reason, women with PCOS will respond just as well to a calorie deficit as healthy women [source].
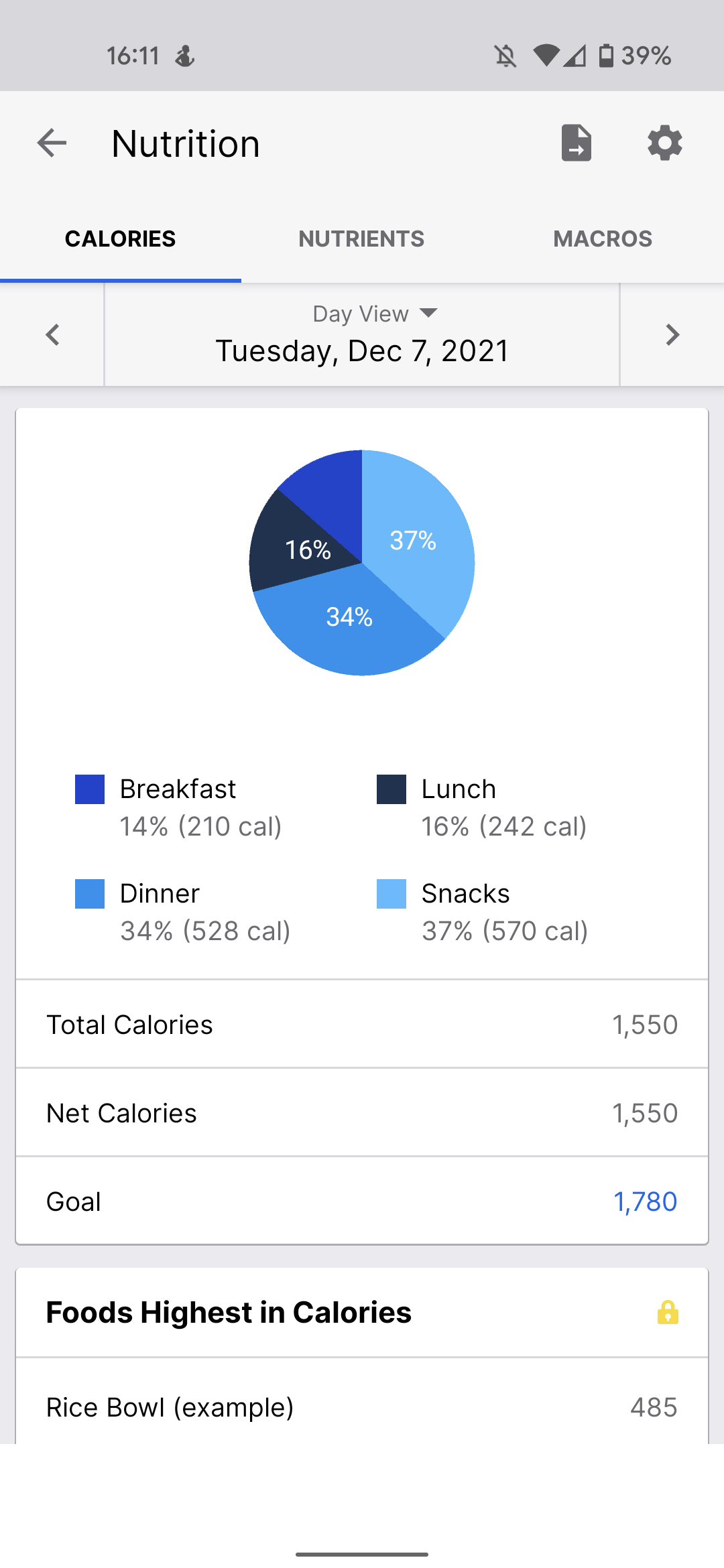
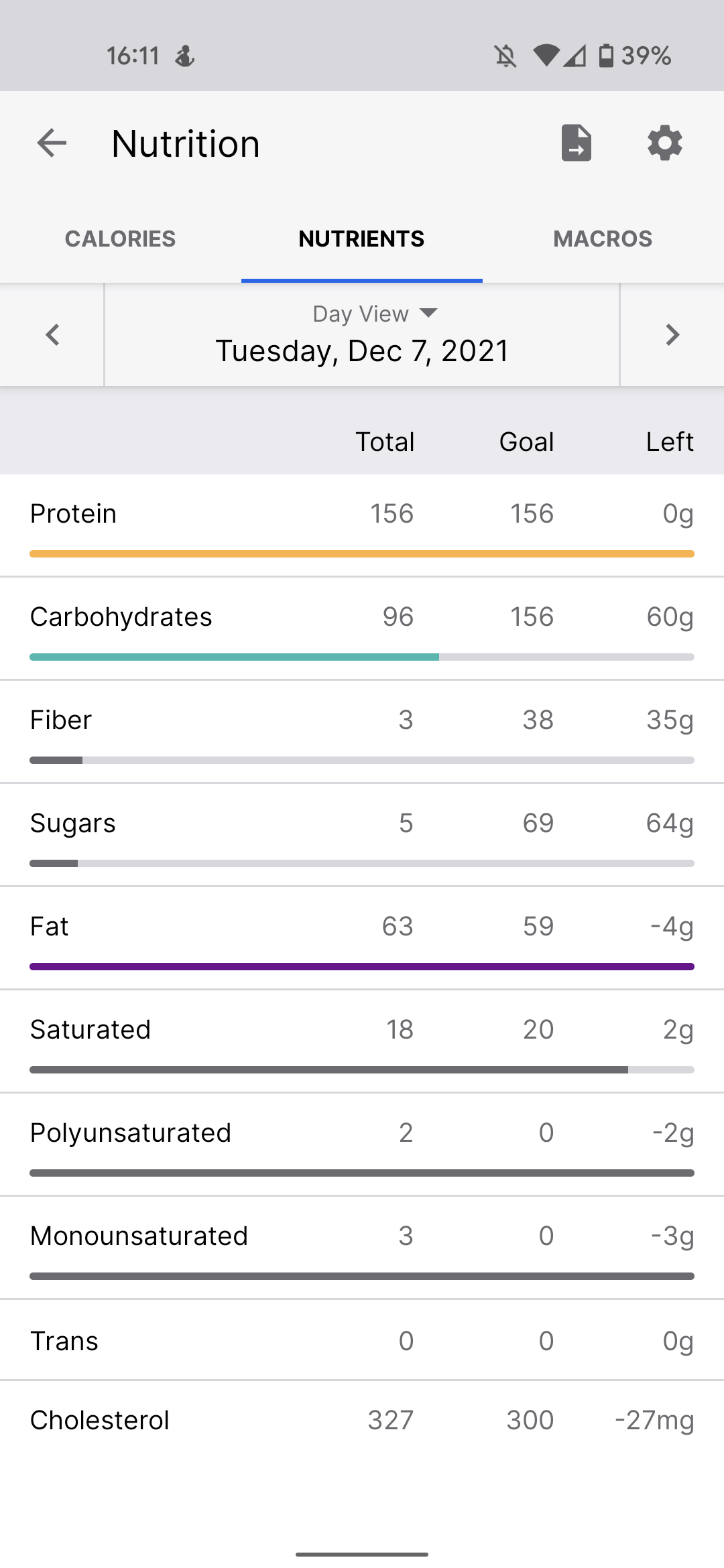
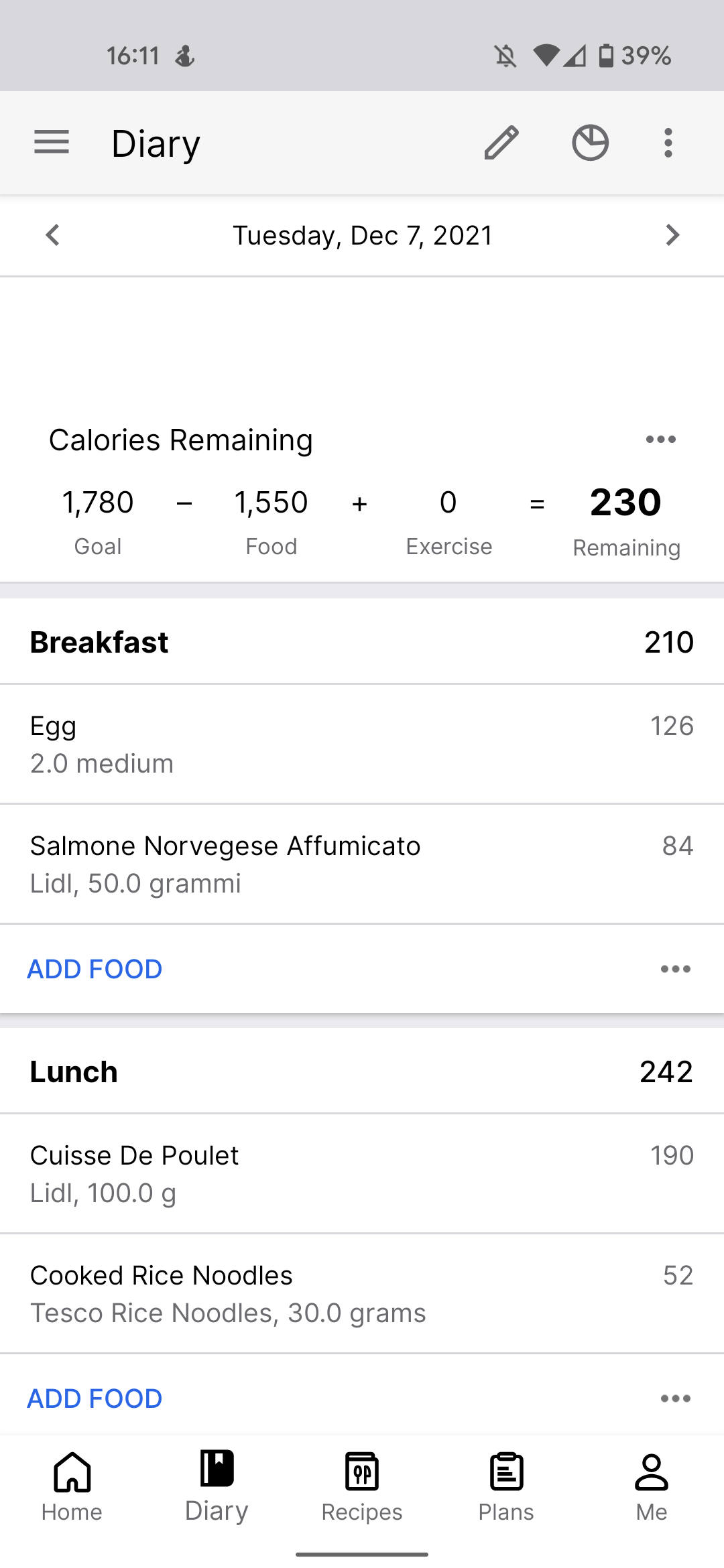
To implement a calorie deficit, start by estimating your daily calorie expenditure. This can be done very easily using a free calculator such as this one. Using your age, weight, height, and activity level the calculator will estimate roughly how many calories you should consume each day to maintain your current weight. Subtract 500 calories from that number and you have your target caloric intake per day. You can then easily monitor your daily calorie intake using a free nutrition tracking app such as myfitnesspal. Maintain this until you reach you desired weight and then recalculate your maintenance level and increase your calorie intake to make sure you don’t lose too much weight.
Mediterranean Diet for PCOS
The Mediterranean diet is widely recognised as one of the healthiest dietary models due to its unique characteristics of regular consumption of unsaturated fat, fibre, foods with a low glycaemic index, antioxidants, vitamins, and animal proteins [source]. Many studies have now shown that the Mediterranean diet helps to protect against many insulin resistance related issues, such as obesity, cardiovascular disease, type II diabetes, non-alcoholic fatty liver disease, breast cancer, and kidney disease [source].
The Mediterranean diet actively helps to reduce inflammatory and oxidative stress responses, improves levels of fat and cholesterol in the blood, improves insulin sensitivity and helps to prevent blood clots [source].
Considering how closely related PCOS is to obesity, insulin resistance and chronic inflammation, it is unsurprising that the Mediterranean diet has been shown to be one of the single best nonpharmacological strategies to treat PCOS.
Studies have compared body composition, PCOS severity and adherence to the Mediterranean diet. They found that typically, women with PCOS have low consumption of olive oil, legumes, fish, and nuts compared to healthy women, but they consumed higher levels of simple carbohydrates, saturated fatty acids, and total fats. Women with PCOS also consumed fewer complex carbohydrates, fibres, and monounsaturated fatty acids. Importantly, testosterone levels correlated with the nutrients mentioned above. Higher levels of simple carbs and bad fats resulted in higher testosterone levels. Lower levels of proteins, complex carbohydrates, fibre, number 3 poly-unsaturated acids, and mono-unsaturated acids all resulted in higher testosterone [source].
“The closer the Mediterranean diet is followed, the better PCOS symptoms are”
Research has shown that the closer women followed the Mediterranean diet, the less severe their PCOS was [source]. Additionally, it has been proven that following the Mediterranean diet can improve ovary health by improving obesity, insulin and testosterone levels [source].
The beneficial effects of the Mediterranean diet have largely been attributed to their high levels of plant polyphenols, found in vegetables, fruit, legumes, grains, nuts, seeds, red wine and extra virgin olive oil. Extra virgin olive oil is considered to be the main health promoting component of the diet due to its incredibly high levels of polyphenols [source]. Polyphenols improve PCOS by reducing inflammation and improving insulin sensitivity. Olive oil also contains high levels of vitamin E and oleic acid, which both help chronic inflammation and have been shown to prevent PCOS related cancers [source]. Lastly, olive oil is rich in resveratrol, which has been proven to reduce testosterone production in PCOS [source].
The downside of the Mediterranean diet is that is much harder to follow for those living outside of the Mediterranean region, due to accessibility of the key ingredients. Despite this, the Mediterranean diet is recognised worldwide for its health benefits and it has been proposed as the best diet to follow to improve PCOS [source].
Ketogenic diet for PCOS.
The ketogenic diet is defined by its high fat and low carbohydrate content. More than 70% of the diet’s calorie intake comes from fats, and excess protein and carbohydrate intake is avoided, resulting in the body producing high levels of ketones. The ketone diet has already been proposed as an effective treatment for several neurological disorders such as Alzheimer’s however there is a growing body of evidence to suggest it is effect for PCOS too [source].
Researchers have noted that the ketogenic diet is effective for treating hormonal and gastric diseases such as type II diabetes and obesity, as well as non-alcoholic fatty liver disease [source]. Studies comparing a ketogenic diet with a normal diet, both using the same amount of calories, found that the ketogenic diet had a 24% higher decrease in blood glucose, resulting in lower insulin secretion and improved insulin resistance, restoring normal insulin function [source]. Most of the benefits of the ketogenic diet for PCOS come from weight reduction, insulin reduction and the resulting testosterone and LH/FSH improvements in women with obesity and PCOS [source].
Several studies following women with PCOS on the ketogenic diet have found improvements in almost all PCOS markers and symptoms [source]. These results seem to suggest that the ketogenic diet is good for treating PCOS however it is important to note that although these effects are beneficial in the short term, there are serious concerns about the side effects of the ketogenic diet in the long term, suggesting that it can affect metabolism, inflammation, glucose tolerance and liver health [source]. As PCOS requires long term management, the ketogenic diet may be a more suitable tool for women that need to lose weight and rapidly improve their PCOS, before switching to a safer and more sustainable diet such as the Mediterranean diet. Lastly, it’s important to remember that ketosis can be very difficult to achieve and varies from person to person, so the same diet may not have the same effects in everyone.
DASH diet for PCOS
The Dietary Approach to Stop Hypertension, or DASH diet, is mostly used for lowering blood pressure in people at risk of cardiovascular problems. The diet emphasizes foods with a low glycaemic index, such as fruit, whole grains, nuts, legumes and low fat dairy. The diet avoids foods like refined grains, processed and red meat, sweets and high saturated fats. The diet is recognised for its high levels of fibre, folic acid, potassium, magnesium and other nutrients [source].
Researchers have found beneficial effects of DASH on insulin resistance, inflammation, obesity, type II diabetes, metabolic syndrome, non-alcoholic fatty liver disease, and cardiovascular disease [source]. Its benefits make it an obvious candidate for managing the symptoms and risks of PCOS. Studies of groups of women with PCOS following DASH for 8 weeks found that they showed improved circulating fat and cholesterol levels, reduced fat around the abdominal area, and improved insulin resistance [source]. A 3 month-long study of women with PCOS following DASH found they had improved weight loss, BMI, fat levels, testosterone levels, and levels of sex hormone binding globulin (which helps to remove testosterone from the body) [source].
The benefits suggest that DASH could be an easy and effective diet for managing PCOS through weight loss and improved insulin resistance.
Low-GI diet for PCOS
Low-glycaemic index (GI) diets are diets that acquire most of their carbohydrates from low GI sources. The glycaemic index of a food is an indicator of how much insulin your body will release after eating the food. Low GI foods, such as oats or lentils, cause the body to release lower amounts of insulin when eaten because they are digested, absorbed, and metabolised slowly [source]. High GI foods, such as white bread or sweet drinks, produce a strong insulin response and can directly increase insulin resistance [source]. This evidence suggests that the type of carbohydrate is important for PCOS, even if the total calories are the same.
Research shows that low GI diets are good for improving insulin response, weight loss, and fat and cholesterol levels. They can improve the risk of diseases such as type II diabetes and cardiovascular disease [source].
Low GI diets are becoming more popular for treating PCOS. Women with PCOS have an enhanced dietary GI due to their worse metabolic profile. In other words, women with PCOS already release too much insulin in response to their food, so every food automatically has a higher glycaemic index. This is why lower GI foods are so much more important for women with PCOS.
One research group compared a low GI diet with another diet for women with PCOS. Both diets resulted in the same amount of weight loss, but the low GI diet caused better insulin sensitivity [source] Studies have also shown that low GI diet decreases inflammation in women with PCOS [source]. Interestingly, early research is also suggesting that low GI diets can help protect women with PCOS against endometrial cancer by decreasing the thickness of the endometrium and improving menstrual health [source]. Low GI diets also improve ovulation cycles in PCOS patients struggling with fertility [source]. In particular, low calorie low GI diets are known to be extremely effective for reducing body fat, BMI, ovulation, menstruation and inducing weight loss [source].
One of the key benefits of a low GI diet is that it is very easy to follow, even when combined with low calories! Low GI foods tend to be very satiating and can reduce feelings of hunger. There are also many options for low GI foods, so that diet is not very restrictive, meaning that it is not boring.
Pulse based diet for PCOS
The pulse based diet is very similar to the low-GI diet or the DASH diet, however it places specific emphasis on consumption of pulses such as lentils, chick peas, split peas and beans. Pulses are high in fibre, low in fat, high in quality protein and complex carbohydrates with very low GIs. Pulses are excellent sources of vitamins and minerals like iron, zinc, folate, calcium, magnesium and potassium, which are all important for normal ovary function [source]. Pulses alone, or as part of a low GI diet, have been proven to improve insulin response in humans [source], resulting in better insulin sensitivity. Pulse consumption has also improved cardiovascular risk in women with PCOS [source]. Interestingly, pulses also contain high levels of phytochemicals, saponins and tannins, which all have very strong anti-cancer effects. Pulses have been suggested to be particularly good at preventing endometrial cancer, a serious risk for PCOS sufferers [source].
Low carb diet for PCOS
The low carbohydrate diet consists of diets where the majority of calories do not come from carbohydrates. In these diets, carbohydrates make up less than 50% of all calories but can be as low as 30%. Research has shown that low carb diets can improve insulin resistance, BMI, and cholesterol in women with PCOS [source]. In fact, in some studies insulin resistance was improved to an extent that is comparable to Metformin. However, studies have not found any real difference between low carb diets and other diets for fertility, hormone levels and other symptoms of PCOS [source].
For many women, the low carb diet can be a difficult one to adhere to as it is quite restrictive in what can be eaten. There has been some suggestion that benefits seen from the low carb diet are the same as those seen from the low-GI diet, however the low-GI diet is considered easier to follow.
Which diet should I use for PCOS?
After reviewing 6 promising options for diets to manage PCOS, you may be wondering which one you should pick. The simple answer is the one that is best for you! The diet that you are happiest, and most comfortable using will be the most effective one to manage your PCOS, as you will be able to do it forever.
There is even the possibility to pick and choose your favourite aspects from each diet. For example, a diet that has its basis in the Mediterranean diet with high olive oil intake, has lower levels of carbs using only low GI carbs with plenty of pulses, high levels of fresh fruit, vegetable, and nuts may be highly effective! Make sure that your diet is varied to ensure that there are no vitamin or mineral deficiencies in the diet and employ methods of calorie restriction if your body weight is too high.
Remember, only sustained, long-term diets will be truly effective at managing PCOS and modifying your risk of disease.
What foods should I avoid for PCOS?
As you can tell from the information above, there are some foods that can be considered to make PCOS and its symptoms worse. People with PCOS should avoid foods and additives that tend to cause a strong insulin response, be highly inflammatory, or may directly impact hormone balance.
All of the diets mentioned above which are beneficial for PCOS make an important point of avoiding foods with a high glycaemic index. A high glycaemic index will stimulate a strong insulin response in the body. A strong insulin response can lead to insulin resistance, which leads to excess insulin, and lastly leads to excess testosterone production in the ovaries. Avoiding high GI foods will help your body to improve its glycaemic control, or its response to blood sugar. Minimising extreme insulin spikes helps to improve insulin sensitivity and therefore reduce the amount of excess insulin in your body, ultimately leading to improved PCOS symptoms. Luckily, eliminating high GI foods from the diet is as simple as recognising which foods have a high GI, and reducing or eliminating them from the diet completely.
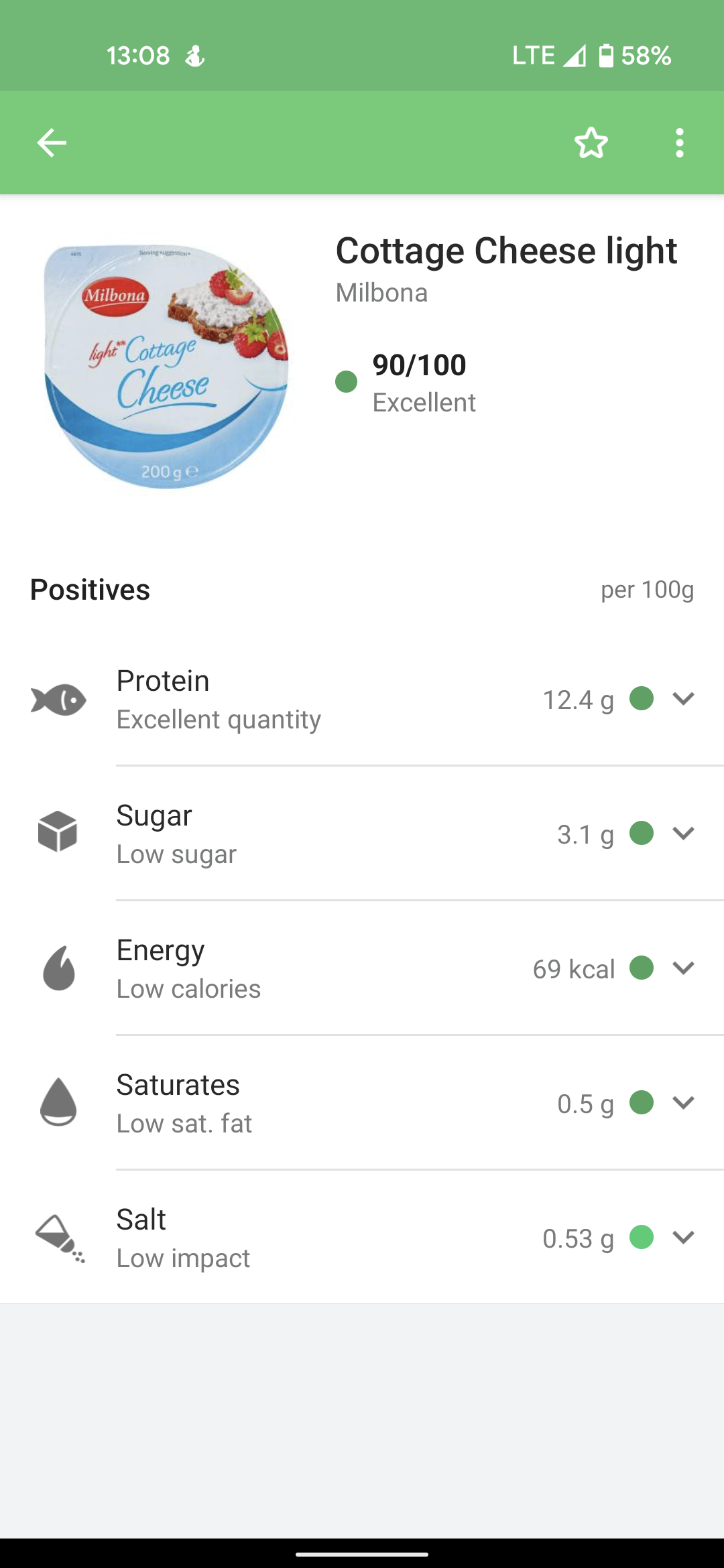
So, how can you identify high GI foods? High GI foods are considered to have a glycaemic index of 70 or over. Low GI foods have a glycaemic index of 55 or less. You can find the glycaemic index of most packaged foods on the label, and you can find the GI of more common foods, like rice or bananas, on google. Alternatively, you can make an estimate of GI using the following descriptions. In general, foods that have a high GI are more processed, more refined, and are quick to digest. Carbohydrates tend to have a higher GI. Common examples of high GI foods are breads, rice, fruits, sweetened products like cakes or sweet yoghurts, and potatoes. On the other hand, low GI foods tend to be high in fibre, high in protein, and high in good fats, and low in sugar. Some examples of low GI foods are vegetables, nuts, legumes, and whole dairy.
Inflammatory foods should also be avoided as they can worsen your body’s ability to produce the correct levels of hormones like luteinising hormone and follicle stimulating hormone. Foods that are considered to be highly inflammatory include refined carbohydrates, like breads and pasta, fried foods, like French fries, red meats and processed meats, trans and saturated fat, like lard or margarine, and sweet foods like sweet drinks, cakes, or chocolate. Inflammatory foods should be eliminated from the diet however treating yourself to small amounts of these foods on infrequent occasions may help you to adhere to your normal, healthy diet, so don’t cut them out completely to begin with if it will increase your chance of relapse.
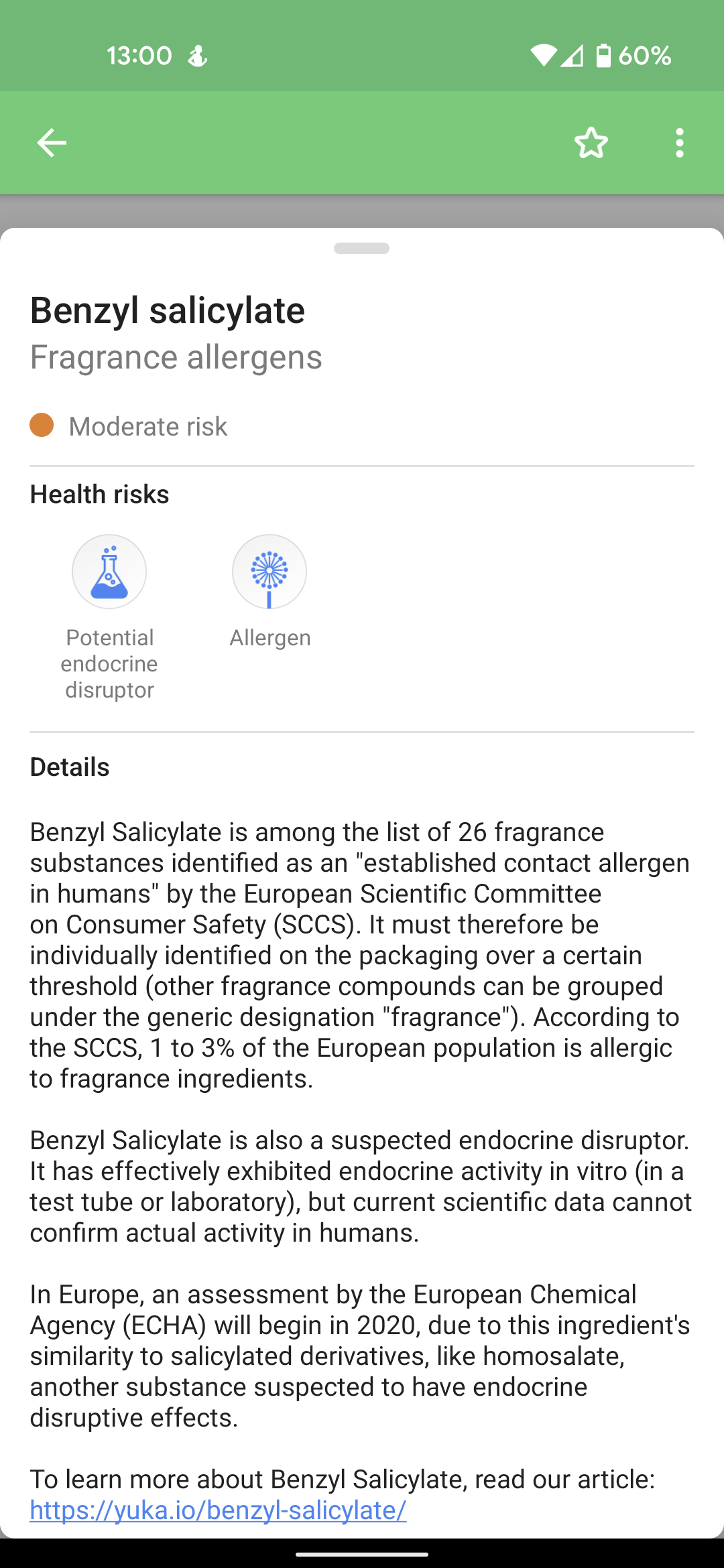
Lastly, foods containing endocrine disrupting chemicals should be avoided as they might directly impact the balance of hormones in your body. A common example of an endocrine disruptor which can be found in food via its packaging and has been strongly associated with PCOS is Bisphenol A, or BPA [source]. Other common disruptors include Phytoestrogens, found in soy and other foods, Dioxins, found in meat, and pesticides. Unlike the previous two categories, these additives are much harder to identify and are often hidden in unlikely foods, even foods that are considered as “healthy” alternatives may contain high levels of these chemicals.
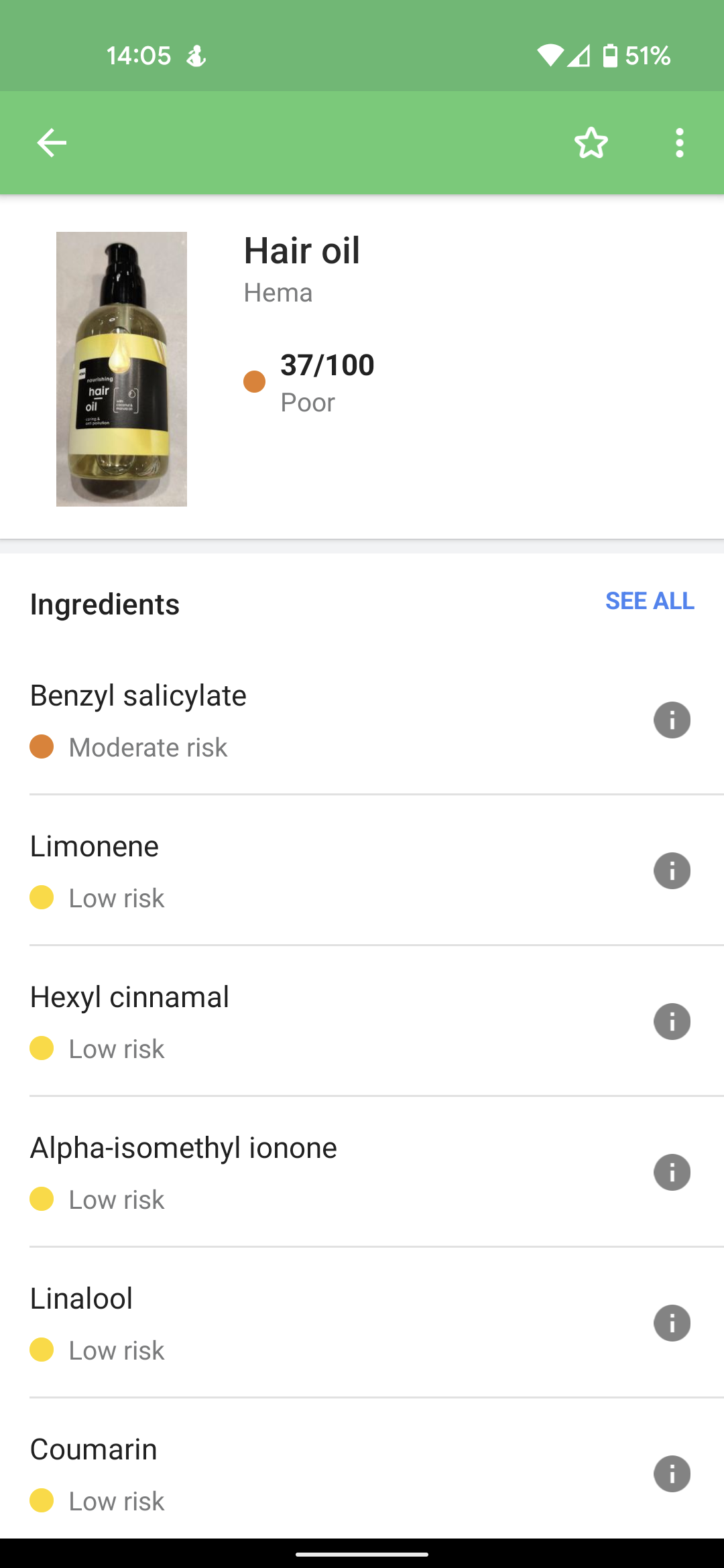
While there is no scientifically suggested method for identifying foods containing these chemicals, many people have found great success with free food scanning apps, such as Yuka. Scanning a food or cosmetic product with Yuka will give you a rating based on several factors such as harmful additives, sugar, protein, fat, salt and fibre content. By selecting the additives you can see all additives in the product, which additives are considered harmful, and if those individual additives cause endocrine (hormone) disruption.
Side note: Our family uses Yuka all the time, we don’t buy any new food or cosmetic products without scanning it first! It’s free and fantastic.